EDI 276 Healthcare Claim Status Request
What is the EDI 276 Transaction Set?
The EDI 276 transaction set and format has been specified by HIPAA 5010 standards for the electronic exchange of the transmission of claims status requests. Health providers use it to verify the status of a claim submitted previously to a payer (e.g., insurance company, HMO, government agencies such as Medicare or Medicaid, etc.). Submitting a 276 status request to the payer is a step in the claim status request/response process.
The payer provides the requested information in response to the 276 Claim Status Inquiry request using the 277 Claim Status Response Transaction Set. An immediate 999 Receipt Acknowledgement may be sent first while the 277 Response follows. Volumes of claim information may be processed with the 276/277 transaction set pair efficiently while meeting HIPAA 5010 requirements.
The EDI 276 A1 transaction set is used by a provider, recipient of healthcare products or services, or their authorized third-party agent to request the status of a healthcare claim or encounter from a healthcare payer.
Note: EDI 276 A1 does not replace the EDI 837 Healthcare Claim Transaction Set but is intended for use after receiving a claim or encountering information. Such a request may occur at the summary or service line detail level.
See how organizations succeed with EDI integration. Check out our X12 EDI case studies.
EDI 276 Claim Status Request in Data Mapper
(Click to enlarge)
EDI 276 Workflow Example
(Click to enlarge)
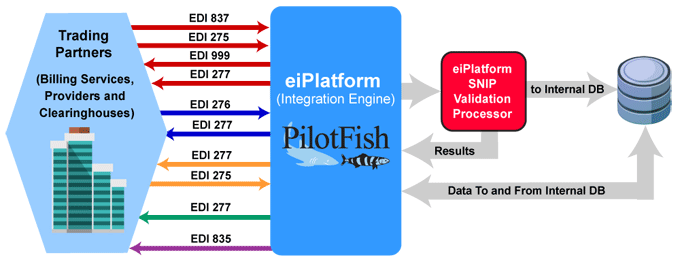
The EDI 276 Claim Status Request is sent to verify the status of EDI 837 claims and/or request additional information from the provider. An EDI 277 Claim Status Response is expected in response.
Providers or third-party services send the EDI 837 Healthcare Claim to payers. The optional EDI 275 Additional Patient Information (Unsolicited) may also be sent with attachments. The payer or clearinghouse system returns an EDI 999 Implementation Acknowledgment to confirm receipt of the incoming EDI 837 Healthcare Claim. The payer may send an EDI 277 Claim Acknowledgement of all claims received in the payer’s pre-processing system.
An EDI 276 Claim Status Request is sent to verify the status of the claim. The EDI 277 Claim Status Response is sent by the payer. The payer may also send an EDI 277 Request for Additional Information. The EDI 275 Additional Information (Solicited) is sent in response and may include patient record attachments.
With aspects of the claim verified, the payer sends the EDI 277 Claim Pending Status Information. The EDI 835 Claim Payment/Advice is used to make payments to healthcare providers and/or provide Explanations of Benefits (EOBs). The EDI 835 is used to detail and track the payment to the claim.
EDI 276 Frequently Asked Questions
Yes, PilotFish supports both real-time and batch processing of EDI 276 transactions. This allows healthcare providers to submit claim status inquiries either instantly for immediate responses or in batches for processing large volumes of inquiries at scheduled times, depending on your operational needs.
Absolutely! PilotFish offers extensive customization options for handling EDI 276 transactions. Users can easily tailor workflows, map data fields, and apply specific business rules to suit their unique needs. Whether you’re a provider, payer, or clearinghouse, PilotFish ensures seamless integration. Check out this healthcare payer case study.
The EDI 276 transaction helps providers track the progress of their claims, reducing the need for manual inquiries and ensuring faster resolution of claim statuses. This improves the overall efficiency of revenue cycle management in healthcare.
PilotFish is designed to scale with your business. It can handle large volumes of EDI 276 transactions efficiently, ensuring high throughput and reliability, whether you are processing thousands or millions of inquiries.
PilotFish ensures compliance with the X12 EDI standards by providing built-in validation tools, including SNIP 1-7, that check the structure and content of EDI 276 transactions before they are processed. This minimizes errors and helps maintain regulatory compliance.
Check out our EDI FAQ pages for more.
EDI 276 A1 Format Example
276 Request Transmission
ASC X12 Version: 005010 | Transaction Set: 276/277 | TR3 ID: 005010X212
The following is a 276 transmission XYZ Services sent to ABC Insurance requesting the status of a set of claims.
Transmission Explanation
| ST*276*0001*005010X212~ |
| BHT*0010*13*ABC276XXX*20050915*1425~ |
| HL*1**20*1~ |
| NM1*PR*2*ABC INSURANCE*****PI*12345~ |
| HL*2*1*21*1~ |
| NM1*41*2*XYZ SERVICE*****46*X67E~ |
| HL*3*2*19*1~ |
| NM1*1P*2*HOME HOSPITAL*****XX*1666666661~ |
| HL*4*3*22*0~ |
| DMG*D8*19301210*M~ |
| NM1*IL*1*SMITH*FRED****MI*123456789A~ |
| TRN*1*ABCXYZ1~ |
| REF*BLT*111~ |
| REF*EJ*SM123456~ |
| AMT*T3*8513.88~ |
| DTP*472*RD8*20050831-20050906~ |
| HL*5*3*22*0~ |
| DMG*D8*19301115*F~ |
| NM1*IL*1*JONES*MARY****MI*234567890A~ |
| TRN*1*ABCXYZ2~ |
| REF*BLT*111~ |
| REF*EJ*JO234567~ |
| AMT*T3*7599~ |
| DTP*472*RD8*20050731-20050809~ |
| HL*6*2*19*1~ |
| NM1*1P*2*HOME HOSPITAL PHYSICIANS*****XX*1666666666~ |
| HL*7*6*22*1~ |
| NM1*IL*1*MANN*JOHN****MI*345678901~ |
| HL*8*7*23~ |
| DMG*D8*19951101*M~ |
| NM1*QC*1*MANN*JOSEPH~ |
| TRN*1*ABCXYZ3~ |
| REF*EJ*MA345678~ |
| SVC*HC:99203*150*****1~ |
| DTP*472*D8*20050501~ |
| SE*36*0001~ |
Source
Accredited Standards Committee X12. ASC X12 Standard [Table Data]. Data Interchange Standards Association, Inc., McLean, VA. ASC X12 Examples
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.