Healthcare Payment Integrity Innovators Deliver for Payers
Over a quarter of the $1 trillion of healthcare administrative spending is wasted as health insurers and providers are 10 to 15 years behind the technology transition. The area is desperate for new approaches. Rapid growth of the payment integrity function across the nation’s health plans has been one response. This health tech entrepreneur innovated a hybrid, cloud-based central platform for healthcare payers to run critical operations at lower cost and increased efficiency as well as deliver better member experiences. The firm partnered with PilotFish to further scale its architecture, support its growing portfolio of solutions and drive interoperability.
THE CLIENT
The healthcare tech entrepreneurs leading this firm leveraged deep technology and product expertise to build new, game-changing solutions from the ground up for payers. The firm’s best-in-class payment accuracy product brings programs in-house and helps health insurance companies gain total control over processes that have been managed by disparate and misaligned vendors. The platform creates efficiencies, saves money as well as frees up payers and providers to focus on delivering care. The solution provides business intelligence by providing robust analytics across claims, lines of business, markets, payments and policies.
THE CHALLENGE
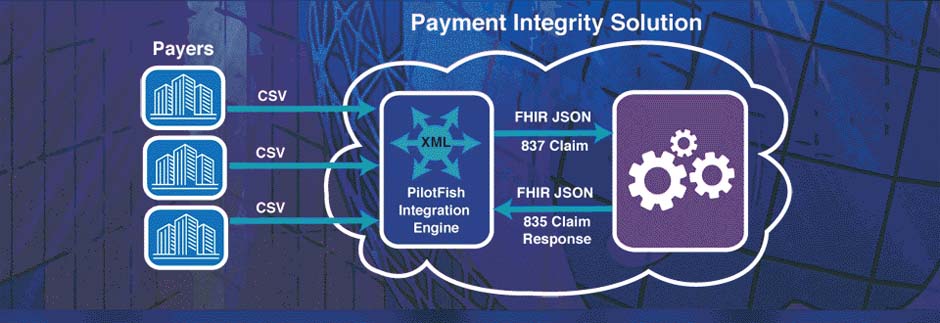
Focusing on the payment accuracy market, the firm’s goal for its payer clients was to achieve the highest value for each administrative dollar spent without sacrificing quality. Payment integrity improvement requires the highest claims accuracy and control of the claims adjustment process. To that end, the platform handles and interrogates healthcare data from disparate internal and external systems, sources and formats. That data must be continuously collected, validated, standardized, transformed and integrated. The firm partnered with PilotFish to effectively solve the many data headaches that face its payer clients by:
- Delivering fast world-class interoperability to healthcare payers
- Integrating efficiently with third-party Core Administrative Processing Solutions (CAPS) widely in use by payers
- Helping to build or supply development tools to tune its architecture to work seamlessly with HL7 FHIR and leverage emerging and proven technologies
THE SOLUTION
Like the client’s platform and portfolio, PilotFish products were developed from the ground up by entrepreneurial leadership with deep technical and product expertise. Each component of PilotFish’s Integration Solution shares a common consistent architecture and design. Virtually any standard can be supported with an identical configuration process.
As the healthcare industry has released X12, HL7 2.x, HL7 3.x, CDA, CCD, CCDA, NCPDP and FHIR, PilotFish quickly and easily added support. And since integrations and process orchestrations are “configured” with no coding required, upgrades are simplified and backward compatibility is maintained.
The client valued the accelerated market leadership it could achieve with the out-of-the-box interoperability brought by PilotFish’s integration software. It entered the Claims Accuracy space delivering advanced FHIR capabilities as well as X12 EDI functionality.
PilotFish provided impressive, robust support for HL7 FHIR with its platform-neutral FHIR API and experience in applying FHIR data models to a wide range of healthcare data and implementations.
PilotFish included specific built-in components for X12 EDI along with comprehensive knowledge of X12 schemas and standards. PilotFish integration software offered a unique level of EDI validation with support for SNIP Levels 1-7. PilotFish also delivered the ability to test every transaction sent or received to validate transaction compliance. These were huge time savers and provided substantial productivity gains.
PilotFish’s Graphical Assembly Line integration approach made FHIR and X12 EDI configurations a virtual breeze for the client’s implementers at all levels, again saving time and money.
With the PilotFish eiConsole for Healthcare and repeatable 7-stage interface assembly line process, users needed only to select from a drop-down menu to read in the desired format. Users simply selected the FHIR version and desired FHIR schema to load the desired subset of the standard and associated inline documentation. The graphical Data Mapper with a FHIR format reader permitted the drag & drop mapping of FHIR documents and X12 EDI transactions.
PilotFish’s powerful lenient parser navigated trading partner variations and dealt with non-compliant data. The lenient parser easily parsed unknown segments and captured data for subsequent conversion and manipulation. The parser also identified, flagged and/or fixed errors, incorrect values, incorrect usages, etc.
Using PilotFish’s Data Mapper to map FHIR “to” and “from” EDI 837 Claims transactions and EDI 835 Remittance Advice messages was incredibly easy and fast as it allowed the client to tower in its entry to the Claims Accuracy space. Goals were met for 100% consistent, accurate and timely claims processing and duly impressed the client’s executive team.
THE BENEFITS
Built with security and compliance top of mind, the client’s platform empowers teams across insurers and providers to work off the same platform with rigorous security controls, a standard in enterprise software. PilotFish provided the client with best-of-breed integration software purpose-built for facilitating the interoperability of disparate systems. PilotFish’s Integration Engine is enhanced to validate FHIR extensions, a key component of implementing FHIR-compliant integration, which is a central concern of the client in growing its customer base.
Armed with extensible software, a forward-thinking approach and the ability to run billions of claims across policies, networks and markets from one platform, the client expects to become the platform of choice to address all aspects of payment integrity – eligibility and verification, prior authorization, pricing and plan optimization and so much more. In partnering with other paradigm-breaking organizations, the firm’s goals of doubling growth year-over-year and developing into a strategic asset are confidently within reach.
Since 2001, PilotFish’s sophisticated architecture and innovations have radically simplified how healthcare integration gets done. Today PilotFish offers the most flexibility and broadest support for healthcare integration of any product on the market and is system, platform and database agnostic. PilotFish’s healthcare integration suite includes support for all healthcare data formats (HL7 2.x, HL7 3.x, FHIR, CCD/CCDA, JSON, XML, X12 EDI, NCPDP, etc.) and communication protocols.
PilotFish is architected to be infinitely extensible with our Open API and flexible to meet any integration requirement. PilotFish distributes Product Licenses and delivers services directly to end users, solution providers and Value-Added Resellers. To learn more, visit our Case Studies or specific solutions like HL7 Integration or X12 EDI Integration.
PilotFish Healthcare Integration will reduce your upfront investment, deliver more value and generate a higher ROI. Give us a call at 813 864 8662 or click the button.
HL7 is the registered trademark of Health Level Seven International.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.