835 Healthcare Claim Payment or Advice Example
What is the EDI 835 Transaction Set?
The EDI 835 Healthcare Claim Payment and Remittance Advice transaction set and format have been specified by HIPAA 5010 standards for the electronic exchange of healthcare payment and benefit information. Healthcare insurance plans use EDI 835 to make payments to healthcare providers and/or provide Explanations of Benefits (EOBs).
When an EDI 837 Healthcare Claim is submitted by a healthcare service provider, the healthcare insurance plan uses the 835 to detail the payment to that claim. What charges were paid, denied, or adjusted; the presence of a deductible, co-insurance, co-pay, etc.; bundling or splitting of claims or line items; how payment was made (e.g. clearinghouse). Healthcare providers use the 835 to track what payments were received for the services they provided and billed.
Note: Multiple 835 transactions may be made in response to one 837. Conversely, one 835 response may be made to multiple 837 submissions. Thus, it is best not to expect a single 835 to match one-to-one with a single 837 as a matter of course.
The EDI 835 W1 transaction set can be used to make a payment, send an Explanation of Benefits (EOB) remittance advice, or make a payment and send an EOB remittance advice. These transactions may be made from a health insurer to a healthcare provider either directly or via a financial institution. Remittance files are used by practices, facilities and billing companies to auto-post claim payments into their systems.
Read about the rapid integration of EDI transactions in our EDI 835 and EDI 837 integration case study for a Solution Provider.
EDI 835 Claim Payment in Data Mapper
(Click to enlarge)
EDI 835 Workflow Example
(Click to enlarge)
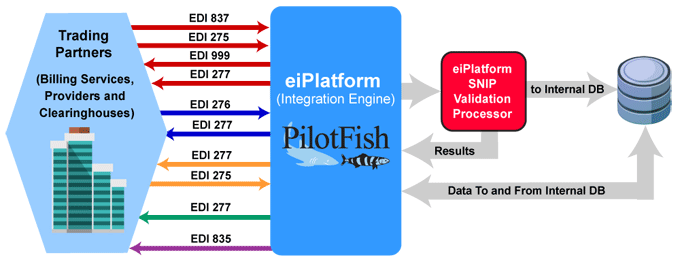
The EDI 835 Claim Payment/Advice is used to make and detail payments to healthcare providers and/or provide Explanations of Benefits (EOBs).
Providers or third-party services send the EDI 837 Healthcare Claim to payers. The optional EDI 275 Additional Patient Information (Unsolicited) may also be sent with attachments. The payer or clearinghouse system returns an EDI 999 Implementation Acknowledgment to confirm receipt of the incoming EDI 837 Healthcare Claim. The payer may send an EDI 277 Claim Acknowledgement of all claims received in the payer’s pre-processing system.
An EDI 276 Claim Status Request is sent to verify the status of the claim. The EDI 277 Claim Status Response is sent by the payer. The payer may also send an EDI 277 Request for Additional Information. The EDI 275 Additional Information (Solicited) is sent in response and may include patient record attachments.
With aspects of the claim verified, the payer sends the EDI 277 Claim Pending Status Information. The EDI 835 Claim Payment/Advice is used to make payments to healthcare providers and/or provide Explanations of Benefits (EOBs). The EDI 835 is used to detail and track the payment to the claim.
EDI 835 Frequently Asked Questions
Pilotfish’s eiConsole Interface Engine can configure interfaces to parse EDI 835 and EDI 837 messages and transform them into SQL inserts. Read more about X12 EDI Parsing.
PilotFish efficiently manages missing data elements for EDI 835 transactions by utilizing comprehensive lookup tables and predefined mappings. Our solution requires specific input data to automate the filling process, ensuring compliance and accuracy in payment information.
Yes, PilotFish allows for customization of the EDI 835 transaction to meet unique payer or provider requirements, ensuring seamless integration into existing systems.
By automating payment remittance and providing detailed payment information, the EDI 835 reduces manual intervention, minimizes errors, and accelerates the payment reconciliation process.
Absolutely. PilotFish expertly conducts SNIP validations, ensuring both integrity and compliance. For example, EDI 835 files that are generated from EDI 837 files. This meticulous validation process not only identifies errors but also presents the findings in a user-friendly XML format. Additionally, users have the flexibility to either generate detailed reports or opt for exceptions based on these validation outcomes.
Check out our EDI FAQ pages for more.
EDI 835 W1 Format Example
Dollars and Data Sent Together
ASC X12 Version: 005010 | Transaction Set: 835 | TR3 ID: 005010X221
Dollars and data are being sent together through the banking system to pay Medicare Part A institutional claims. This scenario depicts the use of the ANSI ASC X12 835 in a governmental institutional environment. The electronic transmission of funds request and the remittance detail are contained within this single 835. In this scenario, one or more Depository Financial Institutions is involved in transferring information from the sender to the receiver. Included are several inpatient and outpatient claim examples.
Transmission Explanation
| ST*835*1234~ |
| BPR*C*150000*C*ACH*CTX*01*999999992*DA*123456*1512345678**01*999988880*DA*98765*20020913~ |
| TRN*1*12345*1512345678~ |
| DTM*405*20020916~ |
| N1*PR*INSURANCE COMPANY OF TIMBUCKTU~ |
| N3*1 MAIN STREET~ |
| N4*TIMBUCKTU*AK*89111~ |
| REF*2U*999~ |
| PER*BL**UR*www.anyhealthplan.com/policies.html~ |
| N1*PE*REGIONAL HOPE HOSPITAL*XX*6543210903~ |
| LX*110212~ |
| TS3*6543210903*11*20021231*1*211366.97********138018.4**73348.57~ |
| TS2*2178.45*1919.71**56.82*197.69*4.23~ |
| CLP*666123*1*211366.97*138018.4**MA*1999999444444*11*1~ |
| CAS*CO*45*73348.57~ |
| NM1*QC*1*JONES*SAM*O***HN*666666666A~ |
| MIA*0***138018.4~ |
| DTM*232*20020816~ |
| DTM*233*20020824~ |
| QTY*CA*8~ |
| LX*130212~ |
| TS3*6543210909*13*19961231*1*15000********11980.33**3019.67~ |
| CLP*777777*1*15000*11980.33**MB*1999999444445*13*1~ |
| CAS*CO*45*3019.67~ |
| NM1*QC*1*BORDER*LIZ*E***HN*996669999B~ |
| MOA***MA02~ |
| DTM*232*20020512~ |
| PLB*6543210903*20021231*CV:CP*-1.27~ |
| SE*29*1234~ |
Source
Accredited Standards Committee X12. ASC X12 Standard [Table Data]. Data Interchange Standards Association, Inc., McLean, VA. ASC X12 Examples
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.