EDI 277 Healthcare Claim Status Notification
What is the EDI 277 Transaction Set?
The EDI 277 transaction set has been specified by HIPAA for the submission of claim status information to respond to a previously received EDI 276 Claim Status Inquiry, to request that a payer provide additional information about a submitted claim (no 276 involved), and for a payer to provide claim status information to a provider via the EDI 277, without having received a 276.
The EDI 277 transaction set is normally used by healthcare payers such as insurance companies, Medicare, third party administrators (TPAs), and clearinghouses in exchanges with providers, recipients, or authorized agents. Information provided in a 277 transaction generally indicates if the claim is Pending or Finalized. If finalized, the transaction indicates the disposition of the claim – rejected, denied, approved for payment or paid. If the claim was approved or paid, payment information might also be provided in the 277, such as method, date, amount, etc. If the claim has been denied or rejected, the transaction may include an explanation, such as if the patient is not eligible.
EDI 277 does not replace the Healthcare Claim Payment/Advice Transaction Set 835. It is not used for account payment posting. The notification may be at a summary or service line detail level.
EDI 277 Claim Status Notification in Data Mapper
(Click to enlarge)
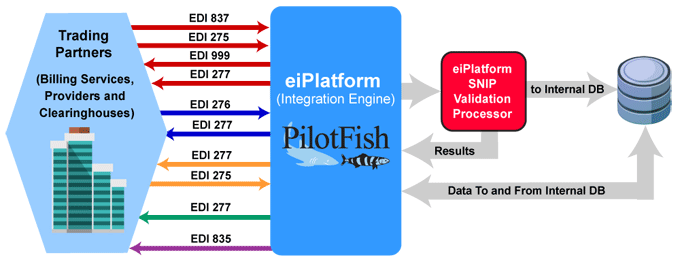
EDI 277 Workflow Example
(Click to enlarge)
An EDI 277 Healthcare Claim Acknowledgment is sent by most payers in receipt of an incoming EDI 837 5010 claim. The EDI 277 Claim Status Response is sent by the payer in response to EDI 276. A solicited or unsolicited EDI 277 Health Care Claim Status Notification may be sent to communicate the status of a claim and/or request additional information.
Providers or third-party services send the EDI 837 Healthcare Claim to payers. The optional EDI 275 Additional Patient Information (Unsolicited) may also be sent with attachments. The payer or clearinghouse system returns an EDI 999 Implementation Acknowledgment to confirm receipt of the incoming EDI 837 Healthcare Claim. The payer may send an EDI 277 Claim Acknowledgement of all claims received in the payer’s pre-processing system.
An EDI 276 Claim Status Request is sent to verify the status of the claim. The EDI 277 Claim Status Response is sent by the payer. The payer may also send an EDI 277 Request for Additional Information. The EDI 275 Additional Information (Solicited) is sent in response and may include patient record attachments.
With aspects of the claim verified, the payer sends the EDI 277 Claim Pending Status Information. The EDI 835 Claim Payment/Advice is used to make payments to healthcare providers and/or provide Explanations of Benefits (EOBs). The EDI 835 is used to detail and track the payment to the claim.
EDI 277 Format Example
277 Response Transmission
ASC X12 Version: 005010 | Transaction Set: 276/277 | TR3 ID: 005010X212
The following is the 277 transmission ABC Insurance sent in response to the 276 transmission from XYZ Service for a set of claims.
Transmission Explanation
| ST*277*0001*005010X212~ |
| BHT*0010*08*277X212*20050916*0810*DG~ |
| HL*1**20*1~ |
| NM1*PR*2*ABC INSURANCE*****PI*12345~ |
| HL*2*1*21*1~ |
| NM1*41*2*XYZ SERVICE*****46*X67E~ |
| HL*3*2*19*1~ |
| NM1*1P*2*HOME HOSPITAL*****XX*1666666661~ |
| HL*4*3*22*0~ |
| NM1*IL*1*SMITH*FRED****MI*123456789A~ |
| TRN*2*ABCXYZ1~ |
| STC*P3:317*20050913**8513.88~ |
| REF*1K*05347006051~ |
| REF*BLT*111~ |
| REF*EJ*SM123456~ |
| DTP*472*RD8*20050831-20050906~ |
| HL*5*3*22*0~ |
| NM1*IL*1*JONES*MARY****MI*234567890A~ |
| TRN*2*ABCXYZ2~ |
| STC*F0:3*20050915**7599*7599~ |
| REF*1K*0529675341~ |
| REF*BLT*111~ |
| REF*EJ*JO234567~ |
| DTP*472*RD8*20050731-20050809~ |
| HL*6*2*19*1~ |
| NM1*1P*2*HOME HOSPITAL PHYSICIANS*****XX*1666666666~ |
| HL*7*6*22*1~ |
| NM1*IL*1*MANN*JOHN****MI*345678901~ |
| HL*8*7*23~ |
| NM1*QC*1*MANN*JOSEPH~ |
| TRN*2*ABCXYC3~ |
| STC*F2:88:QC*20050612**150*0~ |
| REF*1K*051681010827~ |
| REF*EJ*MA345678~ |
| SVC*HC:99203*150*0****1~ |
| STC*F2:88:QC*20050612~ |
| DTP*472*D8*20050501~ |
| SE*38*0001~ |
Source
Accredited Standards Committee X12. ASC X12 Standard [Table Data]. Data Interchange Standards Association, Inc., McLean, VA. ASC X12 Examples
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.