PilotFish Automates EDI 837, EDI 835 and EDI 834 Integration and Cuts Costs
Today, the PilotFish X12 EDI Interface Engine Solution is being leveraged for HIPAA EDI data integration and automation across healthcare. PilotFish’s eiConsole for X12 EDI delivers administrative savings, higher data quality and faster processing of claims (EDI 837), authorizations (EDI 820), benefit enrollments (EDI 834), eligibility requirements (EDI 270/271), acknowledgments (EDI 997/999), payment remittances (EDI 835), analytics, reporting and more.
Automation of X12 EDI HIPAA transactions presents spending and savings opportunities for the entire range of administrative transactions.
But, even though the healthcare industry has moved more quickly toward automation, vast numbers of processes remain partially electronic. That means many unnecessary manual processes still exist.
The greatest opportunity to reduce administrative costs is to focus on eligibility and benefit verification, claim status and remittance advice. Another priority target is prior authorizations.

X12 EDI Interface Quick Tour
Leverage PilotFish to Target EDI 837, EDI 835 and EDI 834 (and any other X12 transaction)
As EDI 834 Benefit Enrollment, EDI 837 Claims Submission and EDI 835 Remittance Advice are ubiquitous in healthcare data exchange, our clients find they are the natural initial targets for improvement. These are transaction processes that our clients, in virtually all areas of the EDI Value Chain, are automating. These include Claims Clearinghouses, Third Party Administrators (TPA), Pharmacy Benefits Managers (PBM), Revenue Cycle Solution Providers, Benefit Administrators, HIEs and more.
With PilotFish’s X12 EDI Interface Engine Solution, our clients have moved forward rapidly to modernize transaction interfaces and integrations, thereby:
- Increasing data quality immediately
- Minimizing manual processes and interventions
- Phasing out legacy systems with little or no pain
- Moving to fully electronic processes
- Reducing administration costs dramatically
PilotFish’s X12 EDI Interface Engine Solution offers fully-featured integrated components built into each stage of the eiConsole’s graphical Automated Interface Assembly Line process. PilotFish’s eiConsole for X12 EDI with its exclusive 3-pane drag & drop Data Mapper is intuitive, visual and understandable with no coding required. And, from end to end, it’s so easy that the majority of interface management and maintenance can be done by business users. With PilotFish, you don’t “discover” burdensome extra charges for additional components.
“Our company is building out all of our healthcare data transactions with the Pilotfish. This includes healthcare X12, NCPDP and various other health care files. The software is easy to learn and allows our team of analysts to implement ETL jobs. The software is very versatile allowing for any file type or connection to data. Unlike some ETL tools, you can build complete platforms to manage your data acquisition and delivery methods“
Director of EDI
Out-of-the-box, PilotFish’s eiConsole for X12 EDI has the capability to read in, parse, validate and transform X12 EDI from any source or trading partner to XML and route the data to any target in any desired format.
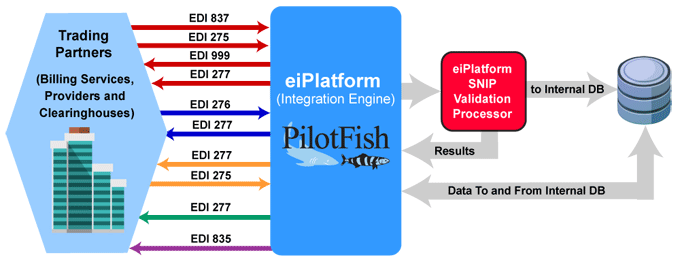
EDI Workflow Example
(Click to enlarge)
Providers or third-party services send the EDI 837 Healthcare Claim to payers. The optional EDI 275 Additional Patient Information (Unsolicited) may also be sent with attachments. The payer or clearinghouse system returns an EDI 999 Implementation Acknowledgment to confirm receipt of the incoming EDI 837 Healthcare Claim. The payer may send an EDI 277 Claim Acknowledgement of all claims received in the payer’s pre-processing system.
An EDI 276 Claim Status Request is sent to verify the status of the claim. The EDI 277 Claim Status Response is sent by the payer. The payer may also send an EDI 277 Request for Additional Information. The EDI 275 Additional Information (Solicited) is sent in response and may include patient record attachments.
With aspects of the claim verified, the payer sends the EDI 277 Claim Pending Status Information. The EDI 835 Claim Payment/Advice is used to make payments to healthcare providers and/or provide Explanations of Benefits (EOBs). The EDI 835 is used to detail and track the payment to the claim.
Single Solution for All of Your EDI Processes and Transactions
Currently, healthcare is experiencing increases in transaction volume in line with the increasing number, types and complexity of health insurance benefit plans. This complexity could very well result in increased manual interventions. In the face of these and future developments, the demand for interoperable administrative and clinical systems only becomes more acute.
PilotFish’s best-of-breed Integration Engine Solution is your EDI integration answer now and in the future. It is architected to be infinitely flexible and extensible. It performs and beats competitors over any use case.
We invite you to take advantage of PilotFish’s eiConsole for X12 EDI by downloading a full, FREE 90-Day Trial Version of our software. Users can try out our EDI Transformation Module and Format Builder.
If you’re curious about the software features, free trial, or even a demo – we’re ready to answer any and all questions. Please call 813 864 8662 or click the button.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.