EDI 270 Eligibility, Coverage of Benefit Inquiry
What is the EDI 270 Transaction Set?
The EDI 270 Healthcare Eligibility/Benefit Inquiry transaction set contains the format and establishes the data contents of the Eligibility, Coverage or Benefit Inquiry Transaction Set specified by HIPAA 5010 standards for electronic data exchange. The 270 inquiry and the 271 response to inquiry transactions are common transaction pairs in healthcare data exchange and compliant with HIPAA 5010 Standards.
The transaction set may be used by all lines of insurance such as Health, Life, and Property and Casualty.
The EDI 270 A1 transaction set is used to inquire about the eligibility, coverages or benefits associated with a benefit plan, employer, plan sponsor, subscriber or a dependent under the subscriber’s policy.
EDI 270 Eligibility Inquiry in Data Mapper
(Click to enlarge)
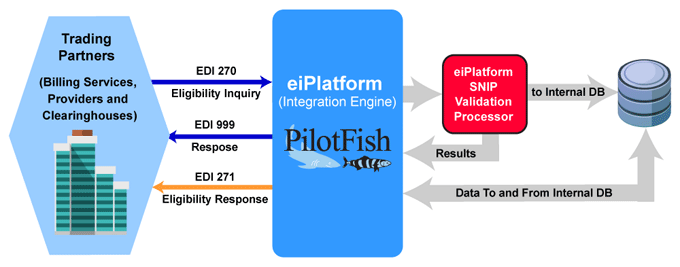
EDI 270 Workflow Example
(Click to enlarge)
X12 EDI 270 Healthcare Eligibility/Benefit Inquiry Workflow
The EDI 270 Healthcare Eligibility/Benefit Inquiry transaction set is sent to inquire about eligibility and/or benefits/coverages for individuals. An EDI 999 Implementation Acknowledgment confirms receipt of the incoming EDI 270. The insurer, sponsor, payor or clearinghouse returns an EDI 271 Healthcare Eligibility/Benefit Response transaction set providing the information.
Explore real-world examples: Read our EDI 270 case studies, including EDI Workers’ Comp Claims Modernized End-to-End in Under a Year.
EDI 270 Frequently Asked Questions
In the PilotFish Data Mapper, EDI messages can be graphically constructed into specific XML representations that the EDI Transformation Module can then convert into properly structured EDI messages.
The EDI 270 transaction set is used for healthcare eligibility inquiries, while the EDI 271 transaction set provides the response with eligibility and benefit information. These transactions help providers verify patient eligibility and coverage before providing services.
Yes, PilotFish is equipped to manage both medical benefit eligibility and pharmacy benefit eligibility (typically part of the X12 EDI 270/271 sets) or any other X12 transaction. Our platform includes robust EDI validation tools and offers specialized expertise in clinical transaction processing.
PilotFish offers a robust, comprehensive validation engine that supports all SNIP levels and provides detailed error reporting. Our solution is highly configurable, integrates easily with existing systems, and includes exceptional customer support to help you navigate any EDI challenges.
PilotFish integrates seamlessly with existing systems through its flexible and scalable architecture. Our solution supports various integration methods, including APIs, web services, and direct database connections, ensuring smooth and efficient EDI validation processes.
Check out our EDI FAQ pages for more.
EDI 270 A1 Format Example
Generic Request by a Clinic for the Patient’s (Subscriber) Eligibility
ASC X12 Version: 005010 | Transaction Set: 270/271 | TR3 ID: 005010X279
This is an example of an eligibility request from a clinic to a payer processed in Real Time. The clinic is inquiring if the patient (the subscriber) has coverage. The request is from Bone and Joint Clinic to the ABC Company. This example uses the Primary Search Option for a subscriber who is the patient and is for a generic request for Eligibility.
Transmission Explanation
| ST*270*1234*005010X279A1~ | Transaction Set ID Code = 270 (Eligibility, Coverage or Benefit Inquiry) Transaction Set Control Number = 1234 Implementation Convention Reference = 005010X279A1 |
| BHT*0022*13*10001234*20060501*1319~ | Hierarchical Structure Code = 0022 (Information Source, Information Receiver, Subscriber, Dependent) Transaction Set Purpose Code = 13 (Request) Identification Reference Identification = 10001234 Date = 20060501 (May 1, 2006) Time = 1:19 PM |
| HL*1**20*1~ | Hierarchical ID Number = 1Hierarchical Parent ID Number = * not used Hierarchical Level Code = 20 (Information Source) Hierarchical Child Code = 1 |
| NM1*PR*2*ABC COMPANY*****PI*842610001~ | Entity Identifier Code = PR (Payer) Entity Type Qualifier = 2 (Non-person) Last Name = ABC Company First Name = * not used Middle Name = * not used Name Prefix = * not used Name Suffix = * not used Identification Code Qualifier = PI (Payer Identification) Identification Code = 842610001 |
| HL*2*1*21*1~ | Hierarchical ID Number = 2 Hierarchical Parent ID Number = 1 Hierarchical Level Code = 21 Hierarchical Child Code = 1 |
| NM1*1P*2*BONE AND JOINT CLINIC*****SV*2000035~ | Entity Identifier Code = 1P (Provider) Entity Type Qualifier = 2 (Non-person) Last Name = Bone and Joint Clinic First Name = * not used Middle Name = * not used Name Prefix = * not used Name Suffix = * not used Identification Code Qualifier = SV Service Provider Number Identification Code = 2000035 |
| HL*3*2*22*0~ | Hierarchical ID Number = 3 Hierarchical Parent ID Number = 2 Hierarchical Level Code = 22 Hierarchical Child Code = 0 |
| TRN*1*93175-012547*9877281234~ | Trace Type Code = 1 (Current Transaction Trace Number) Reference Identification = 93175-012547 Originating Company Identifier = 9877281234 Reference Identification = * not used |
| NM1*IL*1*SMITH*ROBERT****MI*11122333301~ | Entity Identifier Code = IL (Insured or Subscriber) Entity Type Qualifier = 1 (Person) Last Name = Smith First Name = Robert Middle Name = * not used Name Prefix = * not used Name Suffix = * not used Identification Code Qualifier = MI (Member Identification Number) Identification Code = 11122333301 |
| DMG*D8*19430519~ | Date Time Period Format = D8 (Date Expressed in Format CCYYMMDD) Date Time Period = 19430519 |
| DTP*291*D8*20060501~ | Date/Time Qualifier = 291 (Plan) Date Time Period Format Qualifier D8 (Dates Expressed in Format CCYYMMDD) Date Time Period = 20060501 (May 1, 2006) |
| EQ*30~ | Service Type Code = 30 (Health Benefit Plan Coverage) |
| SE*13*1234~ | Number of Included Segments = 13 Transaction Set Control Number = 1234 |
Source
Accredited Standards Committee X12. ASC X12 Standard [Table Data]. Data Interchange Standards Association, Inc., McLean, VA. ASC X12 Examples
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.