Ease of EDI Migration, Stronger Compliance and Reporting
Healthcare payers’ top goals include increasing quality, improving provider relationships and meeting regulatory compliance requirements. With managing costs a consistent issue, increasing interoperability and improving claims accuracy are key to reducing administrative costs. This top-rated Health Maintenance Organization (HMO) and Blue Cross Blue Shield Association (BCBSA) licensee undertook forward-looking initiatives in aligning its business and IT toward common goals by partnering with PilotFish, an industry leader in healthcare integration solutions with extensive experience in payer systems. Immediate challenges for the HMO were to successfully migrate to modern, robust claims processing and strengthen its compliance and reporting infrastructure.
THE CLIENT
The client is a leading Health Maintenance Organization and licensee of the Blue Cross Blue Shield Association. BCBSA is one of the largest health insurance providers in the country, providing coverage to millions of Americans through individual, group and government-sponsored health insurance plans. This top-rated HMO offers individual, family, group and employer coverage plus Medicare Advantage plans. Coverage of medical services is offered through a network of providers. Comprehensive healthcare services include preventive, primary and specialist care, prescription coverage and hospital care. To help members maintain good health, they also offer wellness programs.
THE CHALLENGE
As with other payers, an increasingly complex regulatory environment placed new burdens on the client and presented them with multiple integration challenges. These challenges derived in part from the need to coordinate and streamline a vast array of services, interact with a diverse set of stakeholders and data as well as adhere to numerous regulations and reporting requirements. Their current integration product set lacked modern architecture and built-in functionality to meet current and future business requirements. Not surprisingly, the systems also exhibited performance issues. In short, the HMO was spending too much money for too little ROI.
Compounding these challenges, the client needed to migrate from a legacy integration product being sunsetted and through which all their EDI 837 claims processing was run. In addition, they would be transitioning from another product that had proved to be inadequate in integrating other transaction types. The client accelerated the search for a modern integration solution that offered robust support for EDI as well as the other data formats they worked with now and those they might encounter in the future.
The EDI team (experienced users of EDI) assessed competing solutions for a guarantee of easy, seamless migration from the current EDI 837 claim processing and established workflow. The new solution needed to be performant to handle the increasing number of transactions being processed and the added regulatory reporting requirements. Plus, it had to be easy to use and learn with the expectation that the EDI department would be self-sufficient quickly. When it went live, the payers’ integration solution had to deliver a frictionless experience for all stakeholders, including health plans, providers and members.
THE SOLUTION
The firm partnered with the PilotFish Integration Solution for its industry-leading technology, deep EDI expertise and proven experience in delivering high-performing systems for healthcare payers, including some of the largest in the U.S.
The highest priority for the partnership was immediately addressing the EDI 837 claims processing crisis. X12 EDI 837 Claims is one of the most complex and challenging EDI transactions. Ineffective EDI 837 claims processing could trigger a cascade of expensive problems, including high error rates, inaccurate and inconsistent claims analysis, penalties for regulatory noncompliance and other avoidable costs.
PilotFish’s EDI Integration Solution delivered a complete solution of integrated components and built-in functionality. Designed for ease of use and high efficiency, PilotFish’s unique graphical point-click-drag & drop Automated Graphical Interface Assembly Line approach and visual Data Mapper configures all integrations using the same consistent methodology.
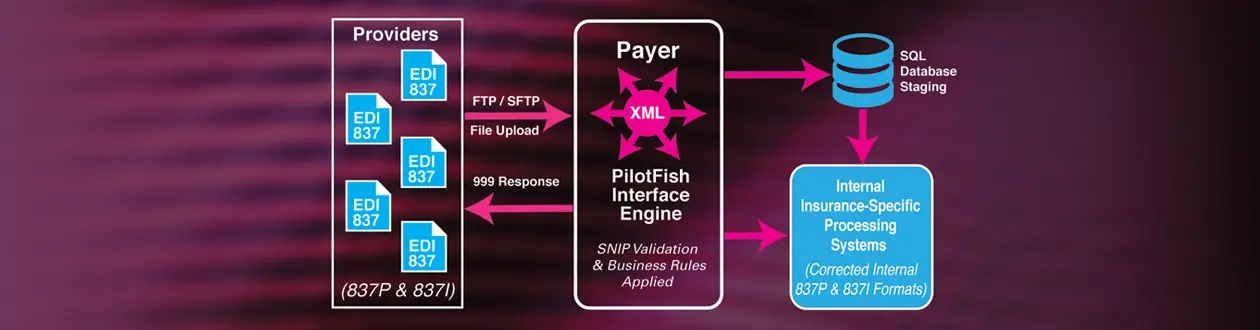
In the client’s EDI 837 workflow, providers received claims in real-time or batch in EDI 837P (Professional) and EDI 837I (Institutional) or other data formats. Claims were downloaded from providers in some cases. File transfers were SFTP. With PilotFish, no current or future scenario presented a problem. PilotFish accepts information in any format (e.g., Excel spreadsheets, PDFs, Word documents, email attachments, JSON, flat files, CSVs, etc.) and via any communication protocol. (More than 25 are built in.)
With PilotFish, 999 Acknowledgements were now automatically generated and sent to submitters.
PilotFish’s X12 EDI integration process includes an EDI Format Builder, which loads a rich data dictionary for EDI transactions, including field-level documentation and friendly field names. The EDI Format Reader provides automatic processes to parse and read in X12 transactions. PilotFish provides SNIP validation out-of-the-box for Types 1-3 and Types 4-7 as an optional add-on.
Rules generated from X12 documentation and HIPAA operate within the EDI SNIP Validation Processor. The SNIP Validation Processor provided a preliminary overall sanity check, saving time. The processor then executed validation rules and external code set testing. The process identified and fixed errors, incorrect values and incorrect usages. Unknown segments and data were captured for subsequent conversion and manipulation.
PilotFish also delivered the ability to test every transaction received or sent to validate transaction compliance.
Each stage of the PilotFish Automated Assembly Line process has a drop-down list of configurable options. Users simply selected the source of the data, connectivity to the source, routing, connectivity and the data format consumable by the target. All incoming data was automatically transformed into an XML representation so that a single open-source W3C language (XSLT) could be used to transform the data. EDI 837P (Professional) and EDI 837I (Institutional) were separated and business rules were applied and further checked for the transactions to be mapped as required for the payment processing stage.
Other processes that previously used a bevy of custom coding and hooks could be done within the graphical Data Mapper. For example, PilotFish now easily assigns a Unique Identifier for each claim within the Data Mapper, which ties back the claim to the audit and other internal tracking databases and payer functions. That eliminated the need for running a separate SQL process. PilotFish also completed external lookups within mappings to update the data before being sent on or loaded.
Claims were mapped back to the 837P and 837I formats to be routed to the receiving adjudication and payment processes where other EDI transactions (EDI 835, EDI 276/277, EDI 275, etc.) were processed. PilotFish now auto-changed ISA, GS and ST data within the mappings to the 837 formats as required by target systems.
PilotFish expeditiously handled virtually any integration requirement, any communication protocol and any data issue encountered. Each benchmark and test of capabilities was met, including necessary report generation.
Seamless migration from its end-of-life legacy EDI claims processing software at every stage was achieved. The IT leadership and the EDI team were impressed with PilotFish as a high-performing, modern single integration system solution – easy to learn, intuitive to use and cost-effective.
THE BENEFITS
The PilotFish suite of integration products enables the integration of Anything to Anything, Anywhere – regardless of operating systems, databases, data formats, communications protocols and security programs.
In this inaugural project and test of capabilities, the marriage of PilotFish’s best-of-breed data transformation and mapping components with X12 standards artifacts delivered not only easy migration but quickly measurable productivity and efficiency gains.
Moving forward, the client plans to take advantage of PilotFish’s unique EDI SNIP 1-7 validation levels by adding SNIP 4 and SNIP 5. With SNIP Type 4, PilotFish validates a much more complete set of semantic rules as defined in the HIPAA X12 EDI implementation guides. For SNIP Type 5, PilotFish validates against 49 external code sets, flags errors for remediation as well as regularly updates and maintains codes.
To advance improvements on the operational level, the client added the PilotFish eiDashboard during the migration initiative. The eiDashboard provides real-time monitoring, operational support and access to data at a granular level for reporting and analytics. They gained immediate insights into transaction processing, including dynamic reporting with data visualization. The eiDashboard also allowed the capture of new data coming through on transactions and the capability to report on them, which supported the growing demands on internal and external reporting.
Next on deck, the HMO is replacing its second integration product, which was inadequate in integrating other transaction types. In this project, the HMO will leverage PilotFish’s support of X12 EDI standards (including all the HIPAA transactions) and all Healthcare standards such as HL7 2.X, 3.X, FHIR, CCD/CCDA, NCPDP, DICOM as well as Positional Flat Files (COBOL), Delimited Files (CSV/Custom), Key/Value, XLS/XLSX, JSON, PDF, Binary (.wav/.jpg) etc. During this transition, PilotFish’s ease of reuse of interfaces and components promises to speed up integrations further while saving the firm money in the near term, with further savings projected.
With its mix of real-time and batch processing, the company is evaluating a move to the PilotFish on-demand licensing model. PilotFish’s on-demand licensing model enables clients to pay for as much PilotFish processing power as needed or used to handle fluctuations in transaction volumes or mostly batch processes.
With PilotFish, the company rapidly achieved benefits in each phase of the claims processing project to transform, modernize and automate processes and workflows. Architected for use by both seasoned software engineers and Business Analysts (BAs), PilotFish delivered the greatest organizational flexibility to the client in the use of scarce IT resources. With PilotFish’s short learning curve, the client was self-sufficient in record time.
Importantly, the partnership with PilotFish immensely strengthened the HMO’s compliance infrastructure, ability to meet evolving regulations, and added reporting requirements.
Since 2001, PilotFish’s sophisticated architecture and innovations have radically simplified how healthcare integration gets done. Today PilotFish offers the most flexibility and broadest support for healthcare integration of any product on the market and is system, platform and database agnostic. PilotFish’s healthcare integration suite includes support for all healthcare data formats (HL7 2.x, HL7 3.x, FHIR, CCD/CCDA, JSON, XML, X12 EDI, NCPDP, etc.) and communication protocols.
PilotFish is architected to be infinitely extensible with our Open API and flexible to meet any integration requirement. PilotFish distributes Product Licenses and delivers services directly to end users, solution providers and Value-Added Resellers. To learn more, visit our Case Studies or specific solutions like HL7 Integration or X12 EDI Integration.
PilotFish Healthcare Integration will reduce your upfront investment, deliver more value and generate a higher ROI. Give us a call at 813 864 8662 or click the button.
HL7 is the registered trademark of Health Level Seven International.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.