Powering the Patient-Centered Medical Home (PCMH)
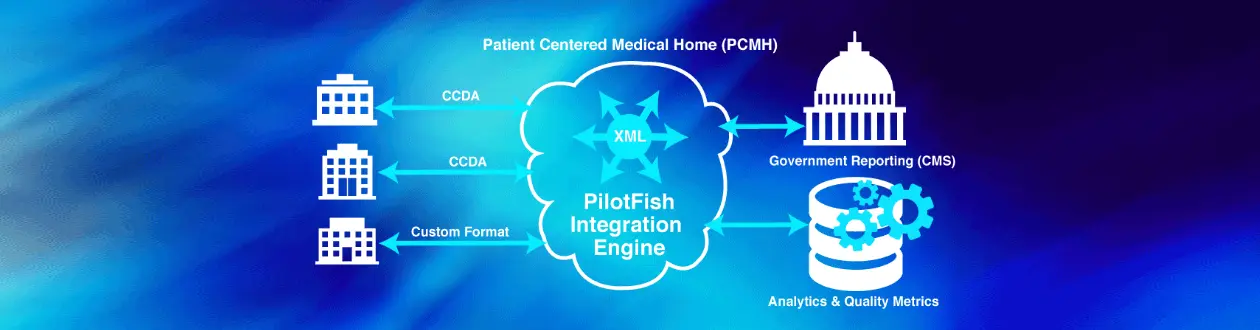
As healthcare transitions away from fee-for-service towards pay-for-performance, reporting and data exchange requirements are also evolving to support this new model of reimbursement. A related set of interoperability challenges is emerging as patients are given increasing control of their healthcare data. Learn how one client has harnessed the power and flexibility of PilotFish to meet these challenges and position itself for the future.
THE CLIENT
The client is a healthcare management organization and a leader in advancing the development and implementation of the Patient-Centered Medical Home (PCMH), as well as other advanced primary care initiatives. It is one of the largest physician groups in Michigan, with more than 1,000 physician members in primary care and specialty fields. The organization is an acclaimed trailblazer in providing services that allow physicians and other providers to develop and sustain high performing independent practices. The organization offers a broad array of infrastructure, technology and clinical services to independent physician practices, mid-level providers, behavioral health professionals and chiropractors who are transitioning to fully integrated, population-based, patient-centric practices to meet health reform mandates.
THE CHALLENGE
The PCMH model is founded on the central patient/physician relationship, with the primary care physician’s office serving as the patient’s “medical home.” The primary care physician’s team coordinates all of a patient’s medical care to improve patient health and outcomes. Care is coordinated and integrated across all elements of the complex healthcare system (e.g., subspecialty care, hospitals, home health agencies, nursing homes) and the patient’s community (e.g., family, public and private community-based services).
Care is facilitated by registries, information technology, health information exchange and other means to assure that patients get the indicated care when and where they need and want it, in a culturally and linguistically appropriate manner. The disparate data that must be integrated to enable personalized, value-based care for patients via the PCMH model may originate from claims and clinical sources such as CSV, Pipe, XML and CCD documents, as well as images and text. For example – in provider-to-provider scenarios, a radiologist may share information with the physician practice. In the provider-to-patient-to-provider scenario, a physician may share test results with a patient and the patient may then schedule a follow-up appointment.
The client supports members in participation in the MACRA Quality Payment Program, which provides “value over volume” Medicare payments to clinicians. The Quality Payment Program rewards the delivery of high-quality patient care through two avenues: Advanced Alternative Payment Models (Advanced APMs) and the Merit-Based Incentive Payment System (MIPS).
MIPS consolidates components of three existing programs – the Physician Quality Reporting System (PQRS), the Physician Value-Based Payment Modifier (PVBM) and the Medicare Electronic Health Record (EHR) Incentive Program for Eligible Professionals (EPs). MIPS continues the focus on quality, cost and use of certified EHR technology (CEHRT) in a cohesive program to avoid redundancies. Additionally, MACRA gives bonus payments to clinicians participating in eligible alternative payment models. The client supplies its PCMH-certified practices the QI reports that CMS requires for providers applying for said payments.
While most will agree that MACRA is complex, its approach is aligned with the Triple Aim of healthcare – better care, healthier people and smarter spending. Much of the information required to produce these quality reports and facilitate PCMH exchange scenarios is provided by EMRs as HL7 CCDA CCDs. CCDA messages contain various types of clinical data expressed across a set of required and optional “templates.” Templates use both unstructured and structured data often referencing specific value sets created from terminology standards such as LOINC, RxNorm and SNOMED.
Aside from the required components, C-CDA documents are “open templates” that may be extended to meet the specific needs of the transmission and/or involved systems. As such, each EMR vendor may configure CCD documents differently. The client was challenged to adapt to and rapidly account for these differences and to be flexible enough to accept data from EMR vendors who may not be able to provide CCD documents and instead send the data in other formats, such as flat files.
Beyond just these differences in message format, the client was required to communicate in a standard, secure fashion dictated by the IHE Profiles for interoperability. As a result, IHE Profiles offer a common framework for vendors and IT departments to understand and address clinical integration needs.
The client selected the PilotFish suite of integration engine solutions to meet its healthcare interoperability challenges and pressing timelines. For those leveraging CCDs or other complex XML formats and dealing with variable data formats, the PilotFish template-based approach to graphical data mapping offers dramatic improvements in productivity over solutions requiring scripting, coding or drawing “spider webs” of interconnecting lines between fields.
THE SOLUTION
The client found it remarkably easy and fast to accomplish EMR integrations using the PilotFish interface engine and tools. While PilotFish always recommends its robust formal training and onboarding program, this client proceeded immediately to implementation without formal training for staff. Using only PilotFish’s Online Documentation Resources and an occasional call to PilotFish professional services, the client’s team implemented 7 new interfaces in less than 6 months including:
- Allscripts – IHE (XDS) profile based integration
- Athena – CCDA ingestion via SFTP
- ModuleMD – CCDA ingestion via SFTP
- eInformatics – Pipe (|) delimited file ingestion via SFTP
- Oaklawn lab – CSV ingestion via SFTP
- Bronson Lab – HL7 ingestion via SFTP
- Oaklawn Hospital (census data – inpatient and ED Visit) – CSV via SFTP
Note: In the first interface, one of the most common IHE Profiles was leveraged. XDS.b Cross-enterprise Document Sharing profile is used for sharing of medical documents between healthcare entities, such as a private physician practice to an information exchange partner. In the PCMH model, this is achieved through a common registry.
Another wrinkle encountered in interface configuration is that while the C-CDA specification provided guidance regarding data encoding for hundreds of CCD fields, it does not require that it be followed. Once each EMR provides the CCDs and allows pushing data into its systems, the challenge of data exchange is still the variability of the data and its structure in the CCDs.
Dealing with incomplete sets of data and documents, slightly incompatible formats or wildly different formats makes it difficult to create valid integrated data. The PilotFish interface engine solution facilitates normalizing such data into a consistent, canonical format and template through a highly productive, repeatable process.
THE BENEFITS
To accelerate integration, the client leveraged PilotFish’s integration software’s flexibility, extensibility, and short learning curve. As this client’s experience attests, creating interfaces via the exclusive “graphical automated interface assembly line” process and open APIs can be done at a fantastic speed, to wit:
- Implementations with new EMRs are now completed in as little as one or two weeks.
- Once an interface is configured – cloning, tweaking it and reusing can be accomplished in 1-2 days.
These technical benefits have delivered a quantifiable return on investment (ROI) for the business. These have been realized through:
- Avoidance of training costs for staff
- Shorter, less costly implementations
- Efficient data exchange out-of-the-box
- The ability to quickly dispatch IHE profiles and workflow interface requirements.
All of the potentials of healthcare coordination are made possible by health registries, health information exchanges and electronic health records (EHRs). By leveraging PilotFish for data normalization and reduced time for integrations, the client has made it easier to quickly evaluate and report on care quality and to create a unified view of the patients’ health picture.
THE FUTURE STATE
The architecture and inherent flexibility of the PilotFish solution will enable the client to adapt and take advantage of new web technologies and standards as they take hold. The client anticipates future regulatory changes that may impact the data reporting requirements that CMS sets forth for Eligible Practices and MIPS participants. With PilotFish in place, such changes will be readily accommodated.
The use of PilotFish also supports instituting more sophisticated and more intuitive Clinical Decision Support (CDS) tools. These tools are gaining traction and technical maturity and, once adopted, will automate specific guidance on patient care to improve community health. These developments translate into an untapped opportunity for health organizations to extend capabilities and investments with a combined technology and information approach.
Going forward, the client may evaluate the utility of the PilotFish eiDashboard. The Dashboard allows monitoring the health of interfaces from high-level message orchestrations all the way down to discrete operations. Its web-based user interface delivers multi-level operational insight of all interface activity. It delivers with significantly reduced downtime and the ability to fix issues on the fly.
With the future-proofed PilotFish integration suite and highly extensible architecture, new client systems will be implemented much more rapidly, minimizing internal resource costs and realizing new revenue opportunities sooner.
Since 2001, PilotFish’s sophisticated architecture and innovations have radically simplified how healthcare integration gets done. Today PilotFish offers the most flexibility and broadest support for healthcare integration of any product on the market and is system, platform and database agnostic. PilotFish’s healthcare integration suite includes support for all healthcare data formats (HL7 2.x, HL7 3.x, FHIR, CCD/CCDA, JSON, XML, X12 EDI, NCPDP, etc.) and communication protocols.
PilotFish is architected to be infinitely extensible with our Open API and flexible to meet any integration requirement. PilotFish distributes Product Licenses and delivers services directly to end users, solution providers and Value-Added Resellers. To learn more, visit our Case Studies or specific solutions like HL7 Integration or X12 EDI Integration.
PilotFish Healthcare Integration will reduce your upfront investment, deliver more value and generate a higher ROI. Give us a call at 813 864 8662 or click the button.
HL7 is the registered trademark of Health Level Seven International.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.