Transforming Healthcare Interoperability: A Seamless Transition to Scalable
Data Integration
The Client, a Medicaid-focused organization, set out to revolutionize its healthcare data integration processes. With an unwavering commitment to improving clinical outcomes and operational efficiency, the company sought a transformative solution to tackle the challenges of healthcare interoperability, Medicaid data integration and scale. They faced pressing issues such as integrating complex healthcare data formats, ensuring EDI compliance automation with industry standards, and streamlining data-sharing workflows. The Client turned to PilotFish to provide the expertise and technology necessary to meet these challenges head-on. The partnership not only addressed immediate needs but also established a scalable foundation for future growth and innovation.
THE CLIENT
The Client, a healthcare solutions organization, operates in the healthcare industry with a clear mission: to support Medicaid providers and payers in delivering high-quality care through data-driven decision-making. As a trusted partner in Medicaid-focused services, they play a vital role in bridging the gaps between disparate healthcare systems, facilitating the exchange of information, and improving the efficiency of care delivery. Their operations are built on the foundation of interoperability, ensuring that healthcare stakeholders—including providers, payers, and state agencies—can access accurate, timely, and actionable data.
The Client works with diverse data sources, including Health Information Exchanges (HIEs), Electronic Health Records (EHRs), Medicaid EDI transactions and FHIR integration frameworks. These systems often contain vast amounts of patient and provider information in a variety of formats, requiring sophisticated integration and transformation capabilities to make the data usable and compliant with healthcare standards. The Client specializes in managing various healthcare transactions, such as patient admissions, discharges, clinical observations, claims processing, and eligibility verifications. By standardizing and streamlining these workflows, they reduce administrative burdens on healthcare providers and enable faster, more accurate decision-making.
At the heart of the Client’s services is a commitment to improving patient outcomes by leveraging data to optimize care coordination and reduce inefficiencies. Their solutions are designed to enable seamless communication between healthcare systems, ensuring that providers have the information they need to deliver the proper care at the right time. For example, their integration capabilities help providers quickly access lab results, update patient demographics, and verify claims, all of which contribute to better care delivery and resource allocation.
The organization’s target audience includes a broad spectrum of healthcare stakeholders. Medicaid providers rely on them to facilitate interoperability between state-run HIEs, EHR systems, and other third-party platforms, ensuring that critical patient data flows seamlessly between systems. Payers depend on them to process claims, validate eligibility, and adhere to stringent compliance requirements, such as SNIP validation and HIPAA standards. State and government agencies also look to the Client to manage Medicaid data exchanges, providing accurate reporting and analytics that inform policy decisions and funding allocations.
With a reputation for innovation and reliability, their solutions are uniquely tailored to the complex demands of Medicaid services. Their ability to manage high transaction volumes, standardize data from diverse sources, and ensure compliance with healthcare regulations positions them as a critical partner for organizations seeking to improve efficiency and scalability. The Client’s dedication to interoperability and its focus on driving measurable improvements in healthcare workflows make it an indispensable player in the Medicaid ecosystem, helping stakeholders navigate the complexities of modern healthcare with confidence and clarity.
THE CHALLENGE
The Client faced a multifaceted set of integration challenges that created inefficiencies, compliance risks, and operational delays. At the core of these issues was the inability of existing tools to handle the complexity and variety of healthcare data formats, including HL7, EDI, and JSON. HL7 messages, such as ADT (Admission, Discharge, Transfer) and ORU (Observation Result), often contained nested and repeating segments that required precise mapping to their SQL database. However, their previous system struggled with maintaining data consistency across disparate sources, which frequently resulted in errors and duplicate entries. Similarly, EDI transactions like the 834 (Benefit Enrollment) and 837 (Healthcare Claim) files presented data transformation and validation challenges, particularly with SNIP-level compliance requirements.
The client faced significant challenges in connecting and managing their healthcare data, which led to inefficiencies, compliance issues, and delays in daily operations. Their existing tools couldn’t handle the variety and complexity of healthcare data formats, such as HL7, EDI, and JSON. For example, HL7 messages like patient admission, discharge, and lab results contain intricate details that must be carefully matched with their database. Unfortunately, their old system often caused errors and duplicate entries when trying to align data from different sources. Similarly, handling EDI transactions like the 834 (Benefit Enrollment) and 837 (Healthcare Claim) files was problematic because their tools struggled with transforming and validating the data to meet strict SNIP-level compliance standards.
Adding to the complexity, the organization’s workflows relied heavily on manual processes to validate and transform data. For example, large datasets often required manual intervention to correct formatting inconsistencies, such as mismatched phone numbers, unstructured addresses, and missing patient identifiers. These inefficiencies consumed valuable time and introduced a greater risk of errors. What they needed was a solution that could automate these workflows while ensuring the highest levels of data accuracy.
Furthermore, the organization was under pressure to meet tight compliance deadlines. For instance, they were required to integrate HL7 data from the State’s Health Information Exchange (HIE) and transform it into their SQL database by June to meet reporting obligations. Any delays in this integration could have led to significant operational and compliance penalties. Additionally, their existing tools were not equipped to handle the high transaction volumes anticipated as their operations scaled, creating concerns about system performance and reliability.
The Client’s technical environment also posed challenges. Their SQL database schema required significant rework to accommodate the hierarchical nature of HL7 data, particularly nested segments like OBX (Observation) and OBR (Order Request). Meanwhile, limitations in server resources, including memory constraints and processing power, further hindered their ability to handle large files and real-time data ingestion. For example, attempts to process files exceeding 50,000 rows frequently resulted in memory errors and system crashes. This left them searching for a solution that could scale to meet their growing data processing needs without overburdening their existing infrastructure.
Finally, the Client’s team needed extensive support to transition from their legacy processes to a more automated and scalable system. They required robust training to build internal expertise in creating data mappings, managing integrations, and troubleshooting errors. Without this foundational knowledge, they risked continued reliance on external resources, further delaying progress and increasing costs.
In selecting a vendor, the organization sought a solution that could address these pain points while providing a consultative approach to implementation. They needed a partner that offered cutting-edge tools, deep expertise in healthcare data integration, and the flexibility to adapt to their specific requirements. PilotFish emerged as the clear choice, offering a suite of tools tailored to handle the complexities of healthcare data and a proven track record of success in the industry.
THE SOLUTION
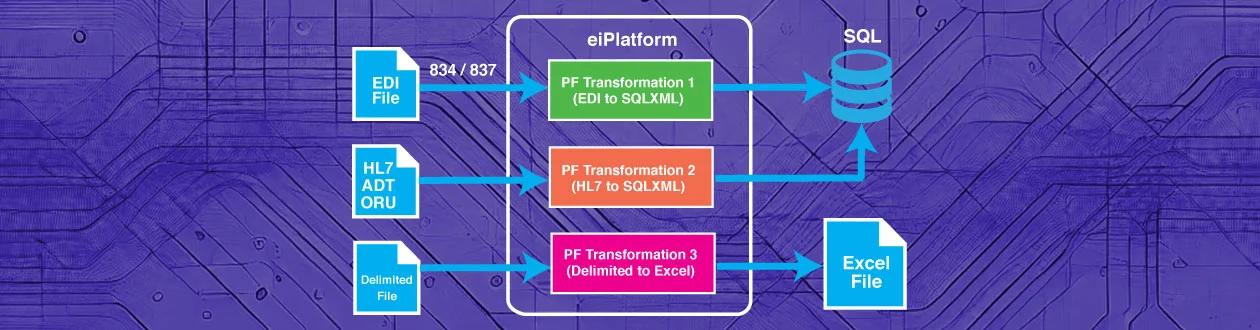
PilotFish’s collaboration with their team began with a thorough assessment of their integration challenges and goals. The solution centered on implementing PilotFish’s interface engine to transform and route complex data formats seamlessly. For example, HL7 messages such as ADT and ORU were transformed into structured SQL database entries, ensuring real-time accessibility for downstream reporting and analytics. PilotFish’s drag & drop data mapper simplified these transformations, enabling the team to create reusable workflows with minimal coding expertise.
The implementation process was deeply collaborative, involving multiple working sessions between PilotFish’s team and the Client’s IT and business units. In these sessions, PilotFish guided them through building and testing critical workflows. For instance, when the Client struggled with integrating complex nested HL7 segments like OBX and OBR, PilotFish worked alongside their team to create dynamic mappings using XSLT. Together, they tested and refined these mappings to ensure accurate data translation and storage, with repeated iterations to handle edge cases and unexpected data structures.
Troubleshooting was an integral part of the implementation. The Client encountered issues such as file path errors, Java heap memory constraints, and discrepancies in data mapping. PilotFish’s team was quick to respond, hosting dedicated sessions to resolve these challenges in real-time. For example, when they faced memory errors during significant file transformations, PilotFish helped them optimize server configurations and adjust memory allocation, ensuring the stability of their workflows. Similarly, PilotFish provided tailored guidance to address FTP connection issues, securely managing credentials through environment variables and testing file transfers to validate end-to-end connectivity.
Training played a vital role in empowering their team to manage their integrations independently. PilotFish delivered comprehensive sessions that combined tool-specific instruction with hands-on problem-solving. These sessions were tailored to the Client’s immediate needs, such as transforming HL7 data into SQL, debugging data mappings, and configuring listeners for real-time data ingestion. The staff were not only trained in using the PilotFish platform but also equipped to troubleshoot issues and make iterative improvements to their workflows.
PilotFish’s support extended beyond implementation, with ongoing collaboration to ensure the solution’s success. Regular check-ins allowed both teams to review progress, address new challenges, and refine processes. For instance, when they needed to rework their database schema to accommodate hierarchical HL7 data, PilotFish provided strategic recommendations on using normalized tables and foreign keys to maintain relational integrity. These iterative efforts ensured that every aspect of the implementation was aligned with their operational goals and technical requirements.
THE BENEFITS
The results of the PilotFish implementation were transformative for the Client, delivering measurable improvements in efficiency, accuracy, and scalability across their operations. By automating previously manual workflows, The Client significantly reduced processing time for large datasets. For instance, files containing over 50,000 rows of data, which previously took several hours to process manually, were now completed within minutes. This automation freed up valuable staff time, allowing The Client’s team to focus on higher-value tasks such as data analysis and strategic planning.
The integration solution also greatly enhanced data accuracy and consistency, a critical need for the Client’s Medicaid-focused operations, including streamlined Medicaid eligibility verification and data submission. PilotFish’s tools ensured inconsistencies, such as varying phone number formats, unstructured addresses, and missing patient identifiers, were automatically resolved during healthcare data validation and transformation. These improvements not only reduced the risk of errors but also ensured that the Client’s data met strict industry compliance standards, including SNIP validation for EDI transactions and HIPAA requirements for data privacy and security. As a result, the Client was able to submit reports and transactions with confidence, knowing they met all regulatory and operational requirements.
The Client’s ability to scale its operations was another significant benefit of the PilotFish solution. Prior to implementation, The Client’s systems struggled to handle high transaction volumes, often leading to delays and system crashes during peak periods. With the PilotFish eiPlatform in place, The Client could now process increasing volumes of HL7 and EDI transactions without any performance degradation. The scalable architecture not only addressed current needs but also provided a robust foundation for future growth. For example, the Client is now positioned to onboard additional healthcare partners and integrate new data sources as their business expands.
The comprehensive training provided by PilotFish to the Client’s internal team equips them with the skills to manage and enhance their integration workflows independently. This self-sufficiency reduced the Client’s reliance on external resources, leading to cost savings and increased operational agility. Team members became proficient in creating and modifying data mappings, troubleshooting errors, and optimizing workflows, ensuring they could adapt to new challenges and requirements without external intervention. The confidence and expertise gained through PilotFish’s training program fostered a culture of continuous improvement within the organization.
The Client’s improved operational efficiency also had a direct positive impact on its healthcare stakeholders. With faster data processing and fewer errors, The Client’s healthcare partners experienced reduced delays in accessing critical information, such as patient demographics, lab results, and claims data. This improved data accessibility enabled providers and payers to make more informed decisions, ultimately enhancing the quality of care delivered to patients.
Looking ahead, the Client is poised to leverage the PilotFish solution to adopt emerging healthcare standards, such as FHIR, and to integrate additional data systems. The flexible and extensible architecture of the PilotFish platform ensures that the Client can seamlessly adapt to evolving industry requirements and technological advancements. This forward-looking capability provides a competitive advantage, enabling the Client to remain at the forefront of healthcare data integration.
The collaborative partnership between PilotFish and the Client also yielded intangible benefits, such as stronger cross-team collaboration and a deeper understanding of integration best practices. Regular working sessions and ongoing support from PilotFish fostered a sense of partnership and shared ownership of the project’s success. The Client’s team consistently praised the responsiveness and expertise of PilotFish’s support staff, who were instrumental in resolving issues quickly and ensuring a smooth transition to production.
Ultimately, the PilotFish implementation transformed the Client’s operations, delivering a robust, scalable, and compliant integration solution that met their immediate needs while positioning them for long-term success. The tangible benefits—reduced processing times, enhanced data accuracy, scalability, and improved compliance—combined with the intangible gains of team strategic adaptability, make this project a benchmark for successful healthcare data integration. The Client is now not only meeting its operational and compliance goals but also exceeding the expectations of its stakeholders, setting a new standard for Medicaid-focused healthcare services.
Since 2001, PilotFish’s sophisticated architecture and innovations have radically simplified how healthcare integration gets done. Today PilotFish offers the most flexibility and broadest support for healthcare integration of any product on the market and is system, platform and database agnostic. PilotFish’s healthcare integration suite includes support for all healthcare data formats (HL7 2.x, HL7 3.x, FHIR, CCD/CCDA, JSON, XML, X12 EDI, NCPDP, etc.) and communication protocols.
PilotFish is architected to be infinitely extensible with our Open API and flexible to meet any integration requirement. PilotFish distributes Product Licenses and delivers services directly to end users, solution providers and Value-Added Resellers. To learn more, visit our Case Studies or specific solutions like HL7 Integration or X12 EDI Integration.
PilotFish Healthcare Integration will reduce your upfront investment, deliver more value and generate a higher ROI. Give us a call at 813 864 8662 or click the button.
HL7 is the registered trademark of Health Level Seven International.
X12, chartered by the American National Standards Institute for more than 35 years, develops and maintains EDI standards and XML schemas.